If you have experienced 3 or more miscarriages in a row, it is called recurrent miscarriage. This is rare and affects 1% of couples. Having a miscarriage can be devastating, but having one after another is often a very traumatic experience. If you have had 3 or more miscarriages in row, you should be referred to a specialist unit dedicated to managing recurrent miscarriage.
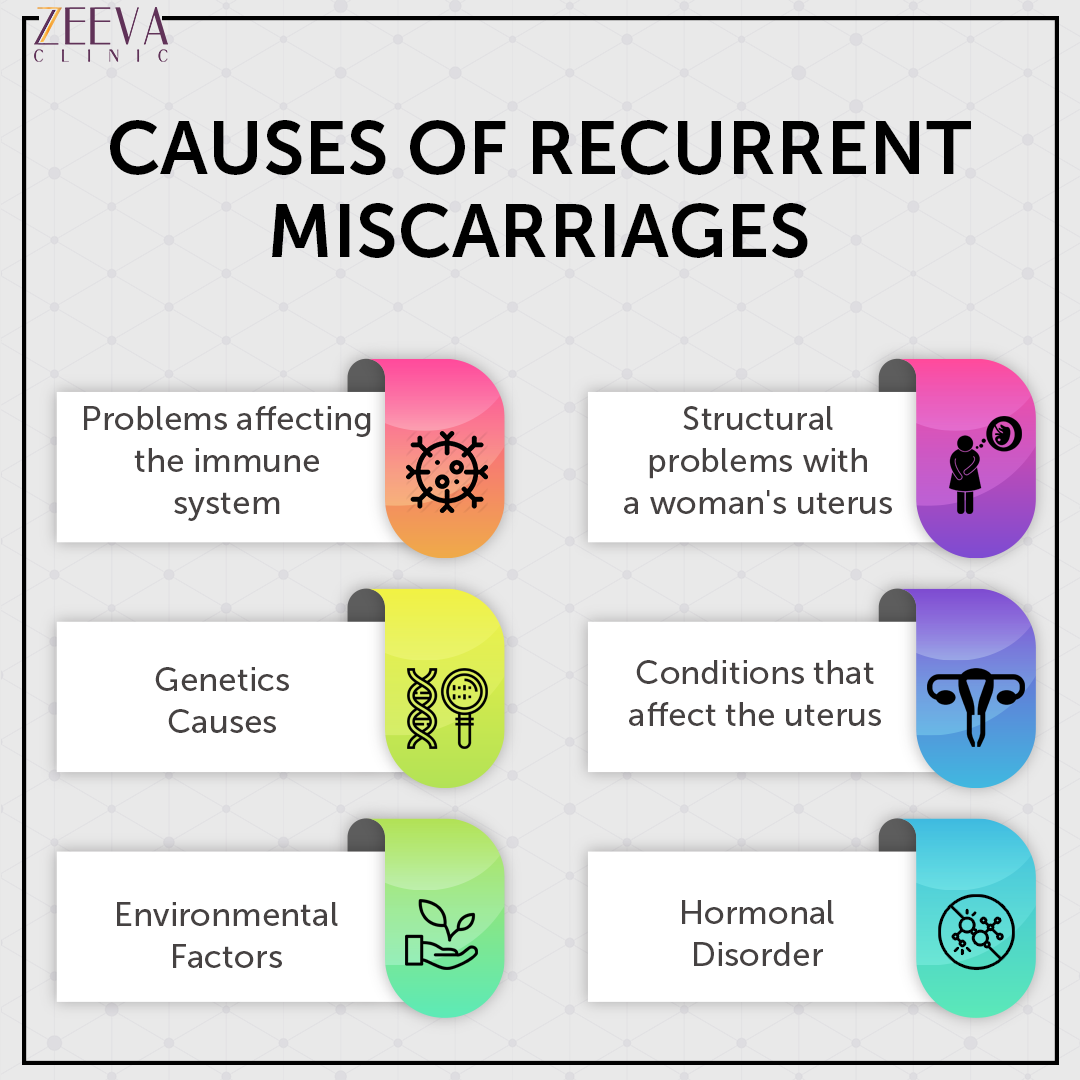
What causes recurrent miscarriage?
There are many possible causes for recurrent miscarriage. Unfortunately, it is not always possible for doctors to find out why it happens. But try to remember that most couples who have had recurrent miscarriage have a good chance of having a baby in the future.
Blood clotting disorders
Some blood clotting disorders, such as systemic lupus erythematosus and antiphospholipid syndrome can cause ‘sticky blood’ and recurrent miscarriage. These rare disorders of the immune system affect the flow of blood to the placenta and may cause clots that prevent the placenta from functioning properly. This can deprive the baby of essential oxygen and nutrients, which may lead to miscarriage. All women with recurrent miscarriage should be screened before pregnancy for antiphospholipid antibodies. Treatment may involve taking aspirin and heparin therapy, which both help to thin the blood. Research shows that in women who have recurrent miscarriage, their blood has an increased tendency to clot, blocking the flow of nutrients to the baby.
Thyroid problems
Thyroid problems have been linked to increased risk of pregnancy loss and other pregnancy complications. They are easy to test for with a blood test and often straight forward to treat. It is important to have a healthy thyroid function before getting pregnant.
Thyroid antibodies
Thyroid antibodies are little molecules in the bloodstream that can attack the thyroid, causing it to not work properly. Having high levels of thyroid antibodies can increase the risk of miscarriage. It is important to check the thyroid function in women who have antibodies, especially when they become pregnant.
Uterine problems
An abnormally-shaped womb can increase your risk of recurrent miscarriage and premature birth. This is usually diagnosed on an ultrasound scan. There are a number of ways to investigate the shape of the uterus and depending on the findings, surgery may be recommended.
Poor Sperm DNA Fragmentation
Current research suggests that the presence of DNA damage in sperm can more than double the risk of miscarriage. This is very significant: until now, miscarriage has mostly been thought of as a female problem. In turn, research into the causes and prevention of miscarriage has focused on women and not on men. DNA Fragmentation
Genetic cause
In a small number of cases, one or both partners may repeatedly pass on an abnormal chromosome, causing recurrent miscarriage. Depending on your miscarriage history, you and your partner may be offered a blood test to check for chromosomal abnormalities (known as karyotyping). If the tests show a problem, you should be referred to a clinical geneticist for further testing.
Cervical weakness
If you have a history of late miscarriages and are considered at risk of cervical incompetence or cervical weakness, you may be offered a scan from 14 weeks to assess the length of your cervix. Depending on your pregnancy and medical history and/or scan findings, you may be advised to have a cervical cerclage (cervical stitch) either before or during a pregnancy.
Natural killer cells
Some experts believe that natural killer cells in the uterus play a part in infertility and miscarriage. It is possible to have tests to measure your level of NK cells. However, it is not available on the NHS. Some fertility clinics offer tests, but not all. If they do, you will have to pay for it. This can be expensive and will vary from clinic to clinic. Find out more about tests and investiations.
Other factors
Age
The risk of miscarriage is highest among couples where the woman is over 35 years of age and the man is over 40.
High number of previous miscarriages
The risk of miscarriage increases after each successive loss (losses one after each other). Women with three miscarriages in a row have a 4 in 10 chance of having another one. This means that 6 out of 10 women (60%) in this situation will go on to have a baby next time.
Tommy’s research into why miscarriage happens
Most parents never find out why their miscarriage happened. Tommy’s believes that parents deserve to be told why their baby has died in pregnancy. As well as ending the cycle of self-blame and guilt, this will improve understanding of the biological processes at work and go towards finding ways to prevent miscarriages not caused by chromosomal abnormalities. This animation shows how we are finding the causes of miscarriage.
What is the care plan after recurrent miscarriages?
Following recurrent miscarriages, you will usually be offered blood tests and a scan to try to identify if there is a problem. Where possible, you will be referred to a specialist unit dedicated to managing recurrent miscarriage. Often, good supportive antenatal care in these circumstances makes a big difference. There is some evidence that attending an Early Pregnancy Unit can reduce the risk of further miscarriages.
Blood tests
Blood tests may be used to check for complications. These include blood clotting disorders, polycystic ovary syndrome and high levels of certain antibodies that can interfere with the pregnancy by affecting the placental blood supply or causing abnormal placental attachment in the womb.
Uterine investigations
An abnormally shaped womb can increase your risk of recurrent miscarriage and premature birth. There are a number of ways to investigate the shape of the uterus and depending on the findings, surgery may be recommended.
Progesterone and recurrent miscarriage
If you have bleeding in your current pregnancy after one or more previous miscarriages, recent research has shown that progesterone can be beneficial. This research (called the PRISM trial) was published in 2019 and showed that the more previous miscarriages, the greater the benefit from progesterone treatment.
Progesterone is a hormone that helps thicken the lining of the womb and helps the mother’s body accept the growing baby. It is given as pessaries (tablets) and taken twice daily in the vagina (like inserting a tampon).
The study that showed that progesterone can be an effective treatment was a large, multi-centre, randomised controlled trial, which is the gold standard of research trials.
Four thousand one hundred and fifty three women with early pregnancy bleeding from 48 hospitals across the UK participated in the study. Around half the women were given vaginal progesterone tablets and the other half were given placebo (dummy) tablets. The findings were:
- For women with no previous miscarriages: the live birth rate was 74% (824/1111) in the progesterone group and 75% (840/1127) in the placebo group, ie no benefit.
- For women who have had 1 to 2 previous miscarriages: the live birth rate was 76% (591/777) in the progesterone group and 72% (534/738) in the placebo group, ie some benefit.
- For women who have had three or more previous miscarriages: the live birth rate was 72% (98/137) in the progesterone group and 57% (85/148) in the placebo group, ie substantial benefit.
The study did not find any safety concern from progesterone treatment.
Talk to your doctor
If you have early pregnancy bleeding and a history of a previous miscarriage, progesterone treatment can be beneficial. As this research is relatively recent, your doctor may not have heard of it, so please discuss this treatment with your GP or the doctors at your local Early Pregnancy Unit. If necessary, show them this information or download this leaflet and bring it with you.
Looking after your emotions
Miscarriage can be devastating. You may be struggling with grief, anxiety and shock, but you do not need to go through this alone. There are lots of organisations that can provide more advice and support.
If you’re worried that you or your partner are struggling to cope after losing a baby, please talk to your GP. They will be able to help you get the support you need.
You can also talk to a Tommy’s midwife for free. You can call them Monday-Friday, 9am-5pm on 0800 0147 800 or you can email them at midwife@tommys.org. Our midwives are trained in bereavement support so will be able to talk to you about what you’re going through.
Reference
Royal College of Obstetricians and Gynaecologists (2011 )The Investigation and treatment of couples with Recurrent First-Trimester and Second Trimester Miscarriage. Green Top Guideline No 17 https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_17.pdf
Coomarasamy et al (2019). A Randomized Trial of Progesterone in Women with Early Pregnancy Bleeding. New England Journal of Medicine.
Royal College of Obstetricians and Gynaecologists. Recurrent and late miscarriage patient information leaftlet. https://www.rcog.org.uk/for-the-public/browse-all-patient-information-leaflets/ recurrent-and-late-miscarriage-patient-information-leaflet/
Information taken from www.tommys.org




0 Comments