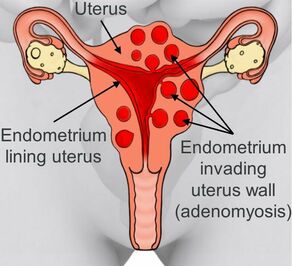
Endometriosis and Adenomyosis both affect the female pelvis but are separate conditions with some similarities and differences. In both conditions, tissue similar to the lining of the uterus, the endometrium, grows in places it shouldn’t. They affect different parts of your body, share some symptoms, and may require different treatments.
You can have both of these problems at the same time. Doctors don’t know exactly what causes them.
Inside vs. Outside: Endometriosis vs. Adenomyosis.
In endometriosis, the same type of cells that line the uterus, or womb, also grow outside of it. The growth can breach nearby organs like your ovaries, fallopian tubes, and bladder. It can make it hard for you to get pregnant.
Adenomyosis, on the other hand, happens when the same kind of cells that line the uterus also grow deep in the muscular wall of the uterus and thicken it.” It doesn’t go past the uterus itself.
Symptoms
Even when the uterine lining grows where it doesn’t belong, it still carries on as usual. It gets thicker and thicker as your monthly cycle nears and then bleeds when your hormones signal that you’re not pregnant. That causes problems.
In endometriosis, it irritates and swells nearby tissues and can lead to scarring. You may notice:
- Belly pain. This is the most common symptom. It may be worse around the time of your period.
- Pain in your back or leg, or pain during or after sex.
- Heavy or painful menstrual bleeding.
- Pain during urination or emptying your bowels.
- Nausea, vomiting, or feeling tired.
Whereas, in adenomyosis, the inside of your womb gets thicker and bigger, which doesn’t usually happen with endometriosis. The enlarged uterus may:
- Put pressure on your bladder and rectum.
- Change the way your uterine muscles tighten (contract)
- Cause heavy and painful periods.
Both conditions can lead to anaemia from menstrual bleeding. This means you don’t have enough iron in your blood. Iron supplements may help.
Causes
Doctors don’t know what causes either endometriosis or adenomyosis. But some things can make them more likely to happen.
Your chances for endometriosis go up if:
- You’re in your 30s or 40s.
- Your mother, sister, or daughter has it.
- You have heavy periods that last more than 7 days.
- Your periods are less than 27 days apart.
- You started your period before you were 11 years old.
Your risk of adenomyosis goes up if you:
- Are in your 40s or older; women diagnosed with adenomyosis tend to be older than those who have endometriosis.
- Have given birth at least once
- Started your periods at age 10 or younger
- Have menstrual cycles that last 24 days or less
Diagnosis of Endometriosis and Adenomyosis.
It can be hard to tell if you have endometriosis or adenomyosis, or both, or something else like fibroids or cysts. Pelvic pain can be caused by many other conditions, including pelvic floor muscle spasm, pelvic infections, and irritable bowel syndrome.
Endometriosis. Sometimes ultrasound can show endometriosis. An MRI also can show larger areas of endometrial tissue outside the uterus, but it could miss smaller patches. The only way to know for sure you have it is with surgery. That way, your doctor can look for endometrial tissue in your belly (outside your uterus). If they see any, small pieces can be taken out for a lab test to confirm the diagnosis.
Adenomyosis. Your uterus may feel bigger than normal and be tender when you push on your belly. An ultrasound or an MRI might diagnose adenomyosis. Sometimes you might not know you have until after a hysterectomy, when your uterine tissue is tested in a lab.
Treatments for endometriosis and adenomyosis.
Endometriosis and adenomyosis usually don’t require treatment unless they cause you problems.
Both may be managed with pain medicines, like non-steroidal anti-inflammatory drugs.
Hormone medicines, such as birth control pills, progestin and progesterone, and gonadotropin releasing hormone agonists, might also be used. These control the way your hormones cycle and can help slow the growth of the endometrial tissue, no matter where it is, but they don’t make it go away. With endometriosis, hormone medicines may help keep new scar tissue from forming.
Gonadotropin-releasing hormone (GnRH) receptor antagonists are another class of hormonal treatments that can be used to treat endometriosis pain.
Several treatments may help control the heavy bleeding from adenomyosis. A special kind of IUD, such as the Mirena Coil, containing hormones, is one option. Others include a procedure to block the supply of blood to the uterus (uterine artery embolisation) or surgery to scar the uterine lining to make your periods lighter (endometrial ablation).
But the only sure cure is a hysterectomy to remove your uterus. You have to be sure you don’t want anymore pregnancies before you decide to have a hysterectomy, embolisation, or ablation.
For endometriosis, surgery might be an option. It can take out the tissue that’s outside your uterus. Scar tissue can be removed, too. If you don’t plan to have more children, your uterus, fallopian tubes, and ovaries can be taken out in a surgery called a hysterectomy with bilateral salpingo-oophorectomy. But even after surgery, there’s a possibility that the pain will return.
Supplements to support both endometriosis and adenomyosis.
Both conditions can be supported with similar supplements. Read Supplements for Endometriosis.




0 Comments