Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that can significantly impact a woman’s fertility. Here’s how PCOS affects fertility:
1. Ovulatory Dysfunction
- Irregular Ovulation: Women with PCOS often have irregular menstrual cycles, which means they may not ovulate regularly or at all. Ovulation is necessary for the release of an egg that can be fertilised by sperm. Without regular ovulation, the chances of conceiving naturally are reduced
- Anovulation: In some cases, women with PCOS experience anovulation, where ovulation does not occur. This is a direct cause of infertility in many women with PCOS.
2. Hormonal Imbalance
- Elevated Androgens: PCOS is associated with higher levels of androgens (male hormones like testosterone). This hormonal imbalance can interfere with the development of follicles, Caption the small sacs in the ovaries where eggs mature. If follicles do not mature properly, ovulation may not occur, leading to infertility.
- Insulin Resistance: Many women with PCOS have insulin resistance, which can lead to higher insulin levels in the body. Elevated insulin can contribute to hormonal imbalances that disrupt ovulation and affect fertility.
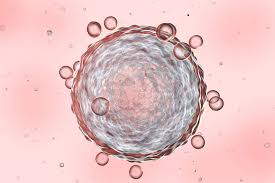
3. Polycystic Ovaries
- Multiple Follicles: The “polycystic” in PCOS refers to the presence of multiple small cysts or follicles in the ovaries. While these are not harmful, they reflect the disrupted ovulation process. Instead of one follicle maturing and releasing an egg, multiple small follicles develop but do not release eggs, further reducing the chances of ovulation and conception.
4. Endometrial Lining Issues
- Irregular Menstrual Cycles: Women with PCOS often have irregular or absent periods, leading to a build-up of the endometrial lining (the lining of the uterus). When this lining eventually sheds, it may not be in sync with ovulation, making it difficult for an embryo to implant properly, thereby reducing fertility.
5. Increased Risk of Miscarriage
- Hormonal Imbalance: The hormonal imbalances in PCOS can also increase the risk of miscarriage. High androgen levels, insulin resistance, and other factors related to PCOS may contribute to a less favourable environment for embryo implantation and development, leading to a higher risk of early pregnancy loss.
6. Treatment and Management
- Lifestyle Changes: Weight management through diet and exercise can improve insulin sensitivity and hormonal balance, promoting regular ovulation and improving fertility
- Medications: Medications like clomiphene citrate (Clomid) are often used to induce ovulation in women with PCOS. Metformin, a medication for insulin resistance, can also be beneficial in improving ovulation.
- Supplements: Supplements such as different types of inositol, Myo-inositol, and D-chiro-inositol can help.
- Inositol is the most heavily researched supplement for PCOS. It’s an important supplement to manage PCOS symptoms, as it’s found to improve insulin-receptor activity and reduce insulin resistance. Those with PCOS have innately lower inositol levels, so supplementation is important.
- Assisted Reproductive Technologies (ART): For women who do not respond to medication, ART like In Vitro Fertilisation (IVF) may be an option.
While PCOS can complicate the process of conceiving, many women with the condition can and do become pregnant with appropriate treatment and management. Early diagnosis and a tailored treatment plan are key to improving fertility outcomes for women with PCOS.




0 Comments