
Semen analysis
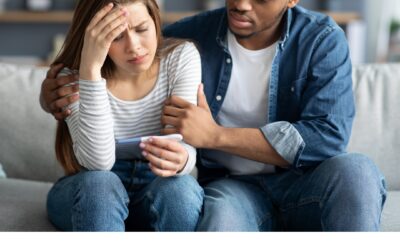
Research now shows that fertility issues are just as likely to be because of an issue with the man(as much as 50% ) as because of an issue with the woman.
If you’re part of a couple having trouble conceiving, it can be very important that the male partner
have a sperm test to understand the possible cause and enable you to move forward in your
fertility journey.
What is a semen analysis?
Semen analysis looks in detail at the sperm count, motility and morphology.
Semen analysis report: What does it mean?
Density
This means your sperm count, that is the number of sperm you have.
Low sperm count is known as oligozoospermia.

Motility
This is the ability of the sperm to swim. Poor sperm motility means the sperm do not swim well
which can mean issues with reaching the egg.
Morphology
This refers to the size and shape of the sperm. Abnormally shaped sperm can be a factor in male
infertility. Low numbers of normal morphology sperm are known as teratozoospermia.
Sperm motility: The ability of the sperm to “swim” to an egg. Progressive motility is the best type
of movement as it means the sperm are moving forward in straight lines.
Lower limit for sperm motility: 40%
Sperm morphology: The way the sperm looks, a morphologically “normal” sperm should have:
- A long tail: made of protein fibers, which helps it “swim”
- A mid-piece: which contains mitochondria (energy-producing organelles) to power the sperm’s movement.
- A nicely shaped head: stores the sperm’s DNA & the acrosomal vesicle (a tiny structure full of enzymes that helps the sperm penetrate the egg by digesting proteins and sugars that make up the zona/shell which surrounds the egg).
Lower limit for normal sperm morphology: 4%
Total sperm count: Total number of sperm within the ejaculate. A high sperm count isn’t helpful to
fertility if most of the sperm have abnormal morphology or can’t swim properly. Similarly, sperm
with textbook morphology may carry abnormal DNA which can negatively impact fertility.
Lower limit for total sperm count: 39million/ejaculate
Sperm concentration: Total number of sperm per milliliter (ml) of ejaculate.
The lower limit for sperm concentration is 15 million per ml.
Lowest values of a “normal” sperm sample
- Semen volume: 1.5 ml
- Total sperm count: 39 million
- Concentration: 15 million per ml
- Total motility: 40%
- Progressive motility: 32%
- Normal morphology: 4%
As per World Health Organisation (WHO 2010)
Please Note!
� one poor Sperm Analysis does not necessarily mean you are infertile
� sperm count & quality can fluctuate so it’s important to repeat testing.
� sperm parameters are affected by a multitude of factors: e.g. illness, stress, lifestyle choices (drugs/alcohol), toxins, etc.
� abstinence length can impact sperm parameters ( between 2-5 days)
� a routine Sperm Analysis cannot measure sperm DNA integrity
� improving sperm health is possible but takes time (about) 74 days for new sperm to develop)

What else might be covered in the Sperm Analysis?
Volume: This is the amount of semen produced and for a sample this needs to be more than 1.5 ml.
For comparison, a teaspoon holds around 5ml.
PH: This refers to how acidic or alkaline the semen is. Semen is ideally between 7.2 and 8 which
makes it slightly alkaline.
Appearance: The lab technicians are looking for anything unusual to the naked eye, the categories
are clear, normal, or slightly clear. Normal is the ideal result.
Viscosity: This means being thick, sticky, and semifluid in consistency. The ideal is normal, but it
could also be classed as highly viscous or slightly viscous.
Liquefaction: This is when the gel formed by proteins from the seminal vesicles break up and the
semen becomes more liquid. It normally takes less than 20 minutes for the sample to change from a
thick gel into a liquid.
Agglutination: This refers to stickiness – what percentage is clumping together.
Aggregation: This is when sperm stick together by head or tails, which can cause issues.
Round Cells: These may be signs of infection – perhaps a previous infection you’re getting over or
a current one. Worth looking into this further if there are more than 1 million cells per ml of fluid.
MAR Test: The test is used to diagnose immunological infertility, which means that anti-sperm
antibodies are present that prevent conception from taking place.
Other terms that may be seen on an analysis :
- Aspermia: absence of semen
- Azoospermia: absence of sperm
- Hypospermia: low semen volume
- Hyperspermia: high semen volume
- Oligozoospermia: very low sperm count
- Asthenozoospermia: poor sperm motility
- Teratozoospermia: sperm carry more morphological defects than usual
- Necrozoospermia: all sperm in the ejaculate is dead
- Leucospermia: a high level of white blood cells in semen
What to do before your test
It’s important to follow these instructions because if you don’t it could mean your test is invalidated or you’ll get an inaccurate result and may need to do it again.
Abstinence
Please abstain from ejaculation for no less than two days and no more than five days before your
appointment.
If it has been less than two days or more than five days since you last ejaculated it could alter the
result
Illness
If you have had a fever or antibiotics recently this could affect your results. Please leave at least one
week after your temperature is back to normal before the appointment.
Please ensure it’s been at least two weeks since you finished any courses of antibiotics. For longer-term therapies, you should wait one month after completion of the medication. If you’re not sure
just check with your clinic.




0 Comments